Exposure and response prevention (ERP) therapy is a specialized form of cognitive behavioral therapy (CBT) that treats obsessive-compulsive disorder (OCD), a complex mental health condition. Unlike other forms of CBT, ERP was specifically designed to break the cycle of obsessions and compulsions, and it’s been clinically proven to significantly reduce symptoms in 80% of people with OCD.
“Exposure and response prevention is really the ‘B’ part of cognitive behavioral therapy,” says Patrick McGrath, PhD, Chief Clinical Officer at NOCD. “It very explicitly focuses on the behavioral aspects of OCD.”
During ERP, you’ll work with a therapist who will gradually expose you to your obsessions and teach you techniques that help you refrain from responding with compulsions. This process is a bit different from traditional talk therapy, as there are components of ERP that require you to put action and intention into stopping compulsive behaviors rather than just talking about them.
“I have never once talked anyone out of OCD, but I sure have behaved people out of OCD,” explains Dr. McGrath. “Exposure and response prevention therapy is a behavioral-based treatment that we use to really behave people out of the influence of OCD.”
Here’s a look into how ERP breaks the OCD cycle, why this form of therapy is so successful at treating OCD, and how you can get started with your own treatment.
How ERP therapy works for OCD
If you have OCD, then you already know how real your fears feel. These obsessions—the intrusive thoughts, images, ideas, sensations, and/or urges—are intense, unwanted, and urgent. They can include doubts about your identity, mental images about harm coming to loved ones, fears about your health, or anything else that seems to go against what you like or believe. What they all have in common is that they create distress—anxiety, fear, doubt, shame, guilt, disgust, or worry.
You may understand that your intrusive thoughts don’t make logical sense, and you may not believe the thoughts that pop into your head. But the thoughts create so much anxiety and distress that the urge to do something about it becomes overwhelming.
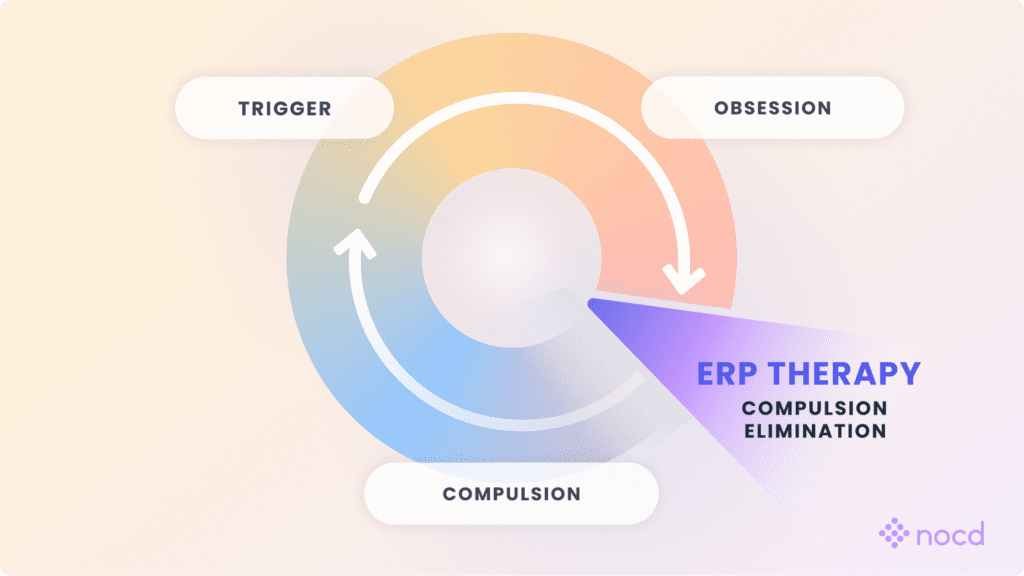
This is where compulsions come in. Compulsions are the physical or mental behaviors you perform to reduce this distress or keep something unwanted from happening. These actions may provide short-term relief from the anxiety caused by obsessions, but they actually make obsessions worse by reinforcing the belief that the obsessions were a threat in the first place. This creates the ongoing cycle of OCD.
The OCD Cycle

“OCD wants you to believe that compulsions will make you feel better or keep obsessions from happening,” shares Dr. McGrath. “But it doesn’t work. Obsessions always come back. In reality, compulsions teach you to run from obsessions, which only gives them more power,” he explains.
ERP disrupts the cycle of OCD by purposely exposing you to these emotional experiences and preventing you from responding to them. “That’s how you ultimately overcome OCD—you teach people that just because they experience an obsession doesn’t mean they have to do a compulsion,” says Dr. McGrath. “When they learn they don’t have to do a compulsion, they typically see fewer obsessions over time because they learn that they don’t have to pay attention to every single thing that pops into their head.”
ERP: A step-by-step guide
Although your individual therapy sessions will be unique to you and your specific OCD symptoms, the following steps can provide a general idea of how it works:
- Identify your fears. “ERP starts with identifying your fears and the areas in your life where you’re doing things that are compulsive,” says Tracie Ibrahim, LMFT, CST, NOCD’s Chief Compliance Officer.
- Develop an exposure hierarchy. You and your therapist will then take your fears and rank them—starting with the ones that cause the least amount of distress to those that are highly distressing.
- Do gradual exposures. With support from your therapist, you’ll slowly and gradually expose yourself to your triggers, starting with the least distressing ones.
- Perform response prevention techniques. Your therapist will teach you strategies that help you refrain from engaging in compulsions when faced with triggers and intrusive thoughts.
- Maintenance. At this point of ERP, you’ll have the tools you need to confront your fears head-on. “You might be doing less exposures, but you’ll also be doing more response prevention. You might see your therapist less and do a lot of this work on your own.”
Because ERP is such a unique and highly specialized form of behavioral therapy, it’s crucial that you work with a therapist who’s not only trained in ERP, but OCD, too—which we’ll cover further in a later section.
Find the right OCD therapist for you
All our therapists are licensed and trained in exposure and response prevention therapy (ERP), the gold standard treatment for OCD.
What are exposures?
Despite popular belief, exposures (aka exposure therapy) are just one-half of ERP. Exposures are anything you can do or experience that triggers your anxiety, fear, or disgust. The purpose of exposures in ERP is to practice intentionally having obsessions, feeling physical sensations, noticing your emotions rising, and experiencing the urges that come with them.
Before you start doing exposures, you’ll work with your therapist to set treatment goals and an exposure hierarchy or fear ladder. “When we’re doing ERP, there are a few things we want to assess first,” explains Dr. McGrath. “We want to get a broad range of things people are afraid of.”
The first stage of treatment is keeping track of your obsessions, triggers and compulsions.
- Obsessions are thoughts, ideas, sensations, images, or urges that may lead you to feel distress, shame, guilt, anxiety, discomfort, etc. that you feel you must neutralize in order to be able to move on in your life.
- Triggers are the situations that cause obsessions to occur.
- Compulsions are all the neutralizing behaviors you do in an attempt to feel better or keep something “bad” from happening. Compulsions can be physical or mental.
After identifying your triggers and symptoms, you will be guided in organizing your obsessions and triggers into an exposure hierarchy or fear ladder based on how much distress they cause. They’re ranked on a simple scale ranging from 1 (minimal distress) to 10 (extreme distress) using the Subjective Units of Distress Scale (SUDS).
Ibrahim notes that there’s no specific structure for ranking your fears. “There’s no perfect number [of exposures],” she explains. “When we ask you to organize them from 1 through 10, it doesn’t mean you need one for each number. You could have some 1s, 4s, 7s, and then some 10s. You just want to have low, medium, and high exposures.”
Types of exposures
There are three types of exposures your therapist can guide you through: imaginal, in-vivo, and interoceptive exposures.
- Imaginal exposure involves bringing to mind your obsessions or feared situations. These types of exposures can be writing or recording stories that intentionally trigger your anxiety, such as the scenario of a feared thing coming true. Imaginal exposures can be less distressing than real-life exposures, so they are more helpful in the earlier stages of ERP for obsessions that cause significant anxiety. Also, they can work well for obsessions when there’s no way to physically encounter a feared idea or situation.
- In-vivo (real life) exposures are when you encounter feared situations or triggers in real life. “An in-vivo exposure is something you didn’t ask for—it just happens naturally,” explains Ibrahim. “You didn’t ask for it and you didn’t set it up, but there it is. There’s also planned in-vivo exposures where a therapist may ask you to go and do something you’re afraid of and not perform a compulsion after.”
- Interoceptive exposures are performed if you experience panic symptoms, which are physiological, sensory issues related to your OCD. In these exposure exercises, sensory or physical experiences are actively triggered. You may work with your therapist to create physical sensations or visual stimuli. These exposures give you the opportunity to accept these feelings without resorting to compulsions.
What is response prevention?
Exposures alone won’t improve your symptoms, which is why the second component of ERP, response prevention (or ritual prevention), is so important.
Response prevention is when you deliberately refrain from engaging in compulsive behaviors that you typically would do to reduce distress from obsessions or prevent something awful from occurring. “Response prevention—the ‘meat and potatoes’ part of ERP—is where you learn to behave your way out of the OCD trap,” explains Ibrahim. “It’s learning that instead of responding with a compulsion or a safety behavior, you will be responding with a more functional behavior that does not feed into your OCD and make it more intense.”
Using the hierarchy you created with your therapist, you’ll begin by exposing yourself to a lower-level trigger and then focus on response prevention. “We’ll work on the elimination of the safety behaviors: avoidance, reassurance, substance use, distractions, and compulsions,” says Dr. McGrath. “When people get rid of those and learn, ‘Now I can handle that thought or image or urge,’ that lays a really great foundation. Then we go up to the next thing. You keep working up the ladder until you’re doing things that you used to think were so difficult.”
Non-engagement responses
A common type of response prevention technique is non-engagement responses (NERs), which are “things we say that help us live with or lean into the anxiety while allowing the distress and anxiety to naturally pass,” explains Ibrahim. NERs are brief, simple phrases you may say when you encounter someone or something that triggers your obsessions.
Examples of non-engagement responses you might say in response to an intrusive thought might be:
- “I am going to handle being uncomfortable.”
- “I might never know the answer to that.”
- “Anything is possible, but I can’t know for sure.”
In addition to non-engagement responses, other response prevention techniques include:
- Delaying compulsions
- Gradually reducing the frequency of compulsions
- Eliminating avoidant behaviors
- Increasing the time between obsessions and compulsions
- Doing the opposite of your compulsions
- Practicing mindfulness
- Using cognitive diffusion techniques (e.g., using humor to respond to intrusive thoughts)
“The important thing about response prevention is that it’s not escaping,” explains Ibrahim. “You’re not trying to escape or engage because engaging tends to be compulsive. Response prevention can be as simple as just not doing anything—just letting [the obsession] live, acknowledging it’s there, and not judging it.”
Can you do ERP on your own?
You may wonder if you can do ERP on your own. Although response prevention may seem straightforward, having a therapist on board who can offer guidance and steer you in the right direction can be more beneficial than doing it on your own.
“One advantage of meeting with an ERP therapist is that you know that you’re going in the right direction and that you’re utilizing the therapy tools in the right way,” says Dr. McGrath. “And what I mean by that is in ways that are efficient and most helpful to you, without any safety behaviors.”
Response prevention—the ‘meat and potatoes’ part of ERP—is where you learn to behave your way out of the OCD trap. It’s learning that instead of responding with a compulsion or a safety behavior, you will be responding with a more functional behavior that does not feed into your OCD and make it more intense.
Tracie Ibrahim, LMFT, CST
How ERP works: Habituation and inhibitory learning
What makes response prevention such a crucial aspect of ERP is habituation and inhibitory learning.
Habituation is the natural process of your brain being able to come down from the distress caused by obsessions without doing compulsions or safety behaviors.
“During habituation, your brain is learning that it doesn’t actually have to be scared or freaked out because the worst-case scenario you thought was going to happen doesn’t happen,” says Ibrahim.
Over time, as you live with the anxiety and discomfort instead of trying to avoid it, that intense feeling gradually fades. This is a key part of ERP because it shows that by facing your fears head-on, you can reduce the power they have over you, making it easier to manage OCD in the long run.
Inhibitory learning is another crucial component of ERP’s effectiveness. “By learning a new way to respond to triggers, it inhibits the recall and occurrence of the former way of responding,” says Dr. McGrath. “Therefore, the performance of the new behavior inhibits the performance of the old behavior.”
How long does ERP take?
The duration of ERP therapy varies depending on the severity of OCD symptoms. However, on average, it can take two months of ERP treatment to see a change in your symptoms. In addition, research reveals that virtual ERP can lead to a significant reduction in OCD symptoms in just 11 hours of therapy.
“Many people feel better even more quickly and may even notice results almost immediately,” says Dr. McGrath. “And some may need a little longer to achieve significant results. People with severe OCD might need elevated care before returning to individual therapy. That could look like an initial residential or partial hospitalization program. Or, perhaps an intensive outpatient program lasting four to six weeks, and then beginning or returning to individual sessions of ERP.”
How long do ERP results last?
As a chronic mental health condition, there’s no cure for OCD, but ERP can make it easier to handle symptoms. “When we talk about a ‘cure,’ it isn’t that you aren’t going to have intrusive thoughts, images, urges, or sensations,” says Dr. McGrath. “You’re going to have them. It’s more about understanding that just because you have them doesn’t mean you need to do something about them.”
While you may not need lifelong ERP sessions, you’ll still use the strategies you learned when triggers and obsessions arise.
“The goal of OCD treatment isn’t to lean on your therapist for life—it’s to eventually become your own therapist, where you’re so skilled at doing ERP that you can manage OCD episodes that pop up,” says Dr. McGrath. “After the severity of your OCD lessens, your therapist should help you find strategies for sustaining your results while slowly reducing how often they see you. For some people, this might take a few months. For others, it may be a few years.”
Once you have the tools to address your obsessions head-on without performing compulsions, you can enter the maintenance phase of your treatment journey. In fact, research reveals that patients who received ERP continued to experience significant improvement in their symptoms that remained up to two years post-treatment.
You have to be patient. [ERP] is not a cure. It’s more like fitness in that you have to put in a lot of time and effort to see results. It’s these incremental changes that compound over time. And, just like fitness, it’s not something you can just do once, and then you’re good–you have to work at it regularly.
Daniel, NOCD Member Advocate
ERP examples for different OCD subtypes
ERP treats all OCD subtypes, which are the subjects that your symptoms revolve around. Some examples of common OCD subtypes include harm, contamination, relationships, and perfectionism. Depending on how your OCD presents, you and your therapist will create ERP therapy exercises that are personalized to address your intrusive thoughts and compulsions.
Here are some examples of how ERP might look for different OCD subtypes:
Obsession: “What if I stab my partner with a kitchen knife?”
Compulsion: Avoiding sharp objects
Response Prevention Technique: Handling sharp objects near others
Obsession: “I’m afraid that if someone who is sick touches me, I’ll get deathly ill.”
Compulsion: Excessive handwashing and/or sanitizing
Response Prevention Technique: Deliberately touching “contaminated” surfaces without immediately washing hands or sanitizing
Obsession: “If the books on my shelf aren’t perfectly lined up, something bad will happen.”
Compulsion: Repeatedly rearranging or aligning items until they feel “just right”
Response Prevention Technique: Purposely leaving books slightly askew or out of order without fixing them
Obsession: “What if my partner is not ‘the one’?”
Compulsion: Seeking constant reassurance from your partner or others
Response Prevention Technique: Working with your partner to agree to no longer answer questions that have been asked and answered
Obsession: “What if I offend God by thinking about something sinful?”
Compulsion: Excessive prayer and/or confession
Response Prevention Technique: Allowing sinful thoughts to be there without trying to neutralize them
Is ERP only used for OCD?
ERP is not just effective for OCD but for other mental health disorders, too. “Most anxiety-related disorders are treated with ERP, like panic disorder, social anxiety disorder, generalized anxiety disorder, or phobia,” says Ibrahim.
According to research, ERP can be effective for treating anxiety and depression if they co-occur with OCD, while 80-90% of people with phobias can also benefit from it.
A specific type of ERP can also help manage post-traumatic stress disorder (PTSD). “There’s a variant of ERP called prolonged exposure that you can use for post-traumatic stress disorder,” adds Dr. McGrath. “There are numerous applications for exposure and response prevention therapy.”
ERP for children and teens with OCD
ERP is delivered almost exactly the same for children and teens as it is for adults with OCD, says Ibrahim. “We just use words that children understand, but everything else is pretty much the same,” she explains. “For example, instead of saying ‘OCD,’ we might talk to children about the ‘worry monster’ or the ‘worry bug.’”
Parents may be included in ERP therapy sessions to ensure they’re not feeding into their child’s OCD. “We always ask for parents’ involvement because most of the time, they’re unknowingly helping keep OCD alive and kicking,” explains Ibrahim. “It’s really important that we’re able to help people know what to do and what not to do.”
ERP and medication management for OCD
In addition to ERP, certain medications are also effective first-line treatments for managing OCD. Selective serotonin reuptake inhibitors (SSRIs), in particular, have a success rate between 40-60% in patients with OCD.
In some cases, medications alone may be enough to treat OCD. However, the combination of medication and ERP can have a stronger effect on reducing the frequency of obsessions and compulsions.
If your therapist recommends adding medication to your treatment plan, it’s crucial that you work with a healthcare provider who specializes in treating OCD. The IOCDF provider directory is a great resource for finding OCD specialists by location. Plus, the 650+ specially trained OCD specialists in the NOCD Therapy directory regularly refer therapy members for medication management with trained providers.
Virtual ERP therapy
A recent study showed that ERP done in live, face-to-face teletherapy is just as effective as in-person ERP therapy. Researchers also discovered that virtual ERP leads to a significant reduction in OCD symptoms and improvements in overall quality of life, depression, anxiety, and stress. Even more, virtual ERP brought these results over twice as quickly as in-person therapy.
The success of virtual ERP comes from how OCD affects us in our everyday environments. Since many obsessions are tied to specific places or situations, doing exposure exercises directly in those spaces can be even more effective than doing them in a therapist’s office. These in-vivo exposures allow you to directly confront your feared triggers in real-life settings. Virtual ERP can even take place outside your home in order to target specific fears and obsessions.
What to look for in an ERP therapist
As you look for an ERP therapist, there are a few things you want to consider to ensure you pick the right clinician to treat your OCD:
- They have training in ERP. Make sure your therapist is specifically trained in ERP so that you’re getting the most effective treatment. While ERP falls under the umbrella of cognitive-behavioral therapy (CBT), not all CBT is effective for OCD.
- They deliver nonjudgmental therapy. A therapist specializing in OCD has heard their patients discuss all kinds of intrusive thoughts and compulsions and will never judge you for yours. They know that these thoughts are not reflective of you or your values—which is exactly why the thoughts are described as intrusive.
- They have experience (or training) working with patients with similar identities to you. You can ask if your therapist has experience working with patients who share similar identities to yours in regard to race, religion, sexual orientation, etc. However, if you can’t find an exact match, it doesn’t mean a therapist can’t help you. “I work with people of all faiths (or lack of), traditions, orientations, and national origins,” says Dr. McGrath. “It is on me to understand their world and help them to find a way to live in it the way they want and not how OCD wants them to.”
“It is okay to interview your therapist and make sure that they’re right for you,” Dr. McGrath adds. “You should make sure that you feel that you’re comfortable working with them, that this is a person who will challenge you, who will listen to you, and you feel as if they have your best interest at heart.”
Bottom line
Exposure and response prevention (ERP) therapy is a specialized, evidence-based treatment that has been proven to be the most effective for reducing OCD symptoms—allowing you to focus more on things that are important to you.
In recent years, many of the barriers to accessing ERP have been significantly reduced, thanks to the introduction of virtual ERP, access to more trained OCD specialists, and more insurance companies covering this type of therapy.
If you’re ready to get your life back from OCD, consider working with an ERP therapist to start your journey to recovery.