Mental health conditions may worsen in the winter due to reduced sunlight and increased isolation, but light therapy may help alleviate some of these effects by boosting serotonin levels and regulating circadian rhythms.
Seasonal affective disorder (SAD), or “winter blues” is a form of depression that usually happens over the course of late fall and winter. Research has shown that the changes in season can affect a number of mental health issues, including anxiety, bipolar disorder, and major depressive disorder. The diminished sense of well-being caused by SAD can also affect symptoms of OCD.
Here’s what you need to know about managing OCD symptoms effectively, and if light therapy, a popular treatment for SAD, could help alleviate some of the seasonal mental health challenges.
Does OCD get worse in the winter?
There are several reasons why winter can impact people’s mental health. They can include reduced sunlight exposure which can disrupt your body’s circadian rhythms—and affect the production of serotonin, a neurotransmitter that contributes to feelings of well-being. Other reasons why winter can be tough on your mental health include lower vitamin D levels, sleep disruptions, isolation, genetic and biological factors, and holidays and special occasions.
Obsessive-compulsive disorder (OCD) is a chronic mental health condition characterized by obsessions, which are recurrent and intrusive thoughts, sensations, images, feelings, or urges that cause anxiety. In response, someone with OCD performs compulsions, which are repetitive behaviors or mental acts that are done to reduce distress, neutralize a thought, or prevent something bad from happening.
“While there is some anecdotal evidence suggesting that symptoms of OCD may worsen for some people during the winter months, the scientific literature on this topic is limited and inconclusive,” explains Nicholas Farrell, PhD, Director of Clinical Development & Programming at NOCD. “One recent paper published in the Archives of Neuropsychiatry found that the severity of obsessive-compulsive symptoms did not show meaningful seasonal changes.
However, the results of this study may not be so simple, according to Dr. Farrell. “The authors noted that people’s subjective well-being varied on a seasonal pattern, worsening in the winter, which is what we would expect. So, there was a general effect but not a specific effect on obsessive-compulsive symptom severity,” he explains. “That said, you might perceive that your obsessions and compulsions get worse in the winter, due to decreased sunlight and reduced access to the sorts of activities that tend to help manage mood and anxiety.”
You might perceive that your obsessions and compulsions get worse in the winter, due to decreased sunlight and reduced access to the sorts of activities that tend to help manage mood and anxiety.
It’s also possible that your OCD gets worse in the winter because of co-occurring mental health conditions like depression, says NOCD therapist Tracie Ibrahim, MA, LMFT, CST. “When your depression is worse, your OCD could get worse, but also when your OCD is worse, your depression could get worse. They feed each other.”
Dr. Farrell adds that certain OCD obsessions may get worse in the winter. For example, fears about inadvertently hitting someone with your car—often referred to as hit-and-run OCD—are likely to intensify when it’s dark at 4 pm and there’s ice on the roads. He also says that fears about having a psychotic breakdown could become heightened when people are more isolated in the wintertime.
“While concrete studies on winter-induced worsening of OCD are sparse, it’s important to recognize the interconnectedness of mental health conditions and how they may be susceptible to seasonal variation,” says Dr. Farrell. “Holistic mental health care should address the broader context of co-occurring disorders and their potential seasonal nuances for comprehensive treatment strategies.”
What is light therapy?
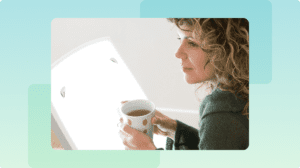
Since the 1980s, light therapy has been used as a treatment for winter-pattern SAD. The goal is to expose people to bright light to compensate for the lack of sunlight. This involves sitting in front of a light box that emits a bright light (similar to sitting out in the sun), for around 20 to 30 minutes every morning.
Research indicates that the therapy helps to regulate your circadian rhythm, which is your body’s internal clock that controls your sleep-wake cycle. Light therapy is also known to boost serotonin, a neurotransmitter in the brain that plays a key role in regulating mood, sleep, and anxiety.
There is mixed evidence regarding the effectiveness of light therapy in the treatment of depression. However, some studies indicate that it is effective for the treatment of SAD.
It’s important to talk to your healthcare provider before starting light therapy—especially if you have bipolar disorder. Increasing exposure too quickly or using the light box for too long may cause manic symptoms. Additionally, if you have eye problems, such as glaucoma, cataracts or eye damage from diabetes, you should consult an eye specialist before doing light therapy.
Does light therapy help with OCD?
There isn’t enough evidence showing that light therapy can treat OCD. However, it can be effective in reducing symptoms of co-occurring mental health conditions, such as depression. In fact, research indicates that between 25 to 50% of people with OCD also meet the criteria for a major depressive episode. OCD can contribute to the development of depression, and in turn, depression can make it more challenging to manage OCD symptoms.
“Light therapy works for SAD,” Ibrahim says. “Just for that. Not for anything else.” With that being said, you can do other things to support your overall mental health, which in turn, can make it easier to manage OCD symptoms.
Light therapy works for SAD—just for that. Not for anything else.
Other natural strategies to reduce the winter’s impact on your mental health include:
- Get regular exercise. Physical activity has been consistently linked to improved mood and reduced symptoms of various mental health conditions. Exercise can enhance the production of neurotransmitters like serotonin, as well as endorphins, a hormone that makes you feel good—both of which can contribute to better emotional well-being.
- Supplement with vitamin D. Adequate vitamin D is essential for overall health and plays a role in mood regulation. Since reduced sunlight exposure in winter can lead to lower vitamin D levels, supplementation of around 2,000 IU daily may be beneficial. But be sure to talk with your healthcare provider to determine the right amount of supplementation for you.
- Be social. Maintaining social connections and engaging with friends and family can be crucial for mental well-being. Staying connected can provide emotional support, reduce feelings of isolation, and offer a sense of belonging during the winter months.
While there’s evidence that these interventions can help alleviate winter’s effect on people susceptible to SAD, the most effective treatment for OCD is an evidence-based approach called exposure and response prevention therapy (ERP), and it can help you recover from symptoms at any time of year.
Evidence-based treatment for OCD
ERP is a specialized form of cognitive behavioral therapy (CBT) that’s designed to treat OCD.
During ERP, you’ll work with a trained therapist to gradually confront your triggers while resisting the urge to perform compulsions.
You’ll begin by creating an exposure hierarchy—a list of the ERP exercises you and your therapist collaborate on ranging from least to most anxiety-provoking. This hierarchy will help you gradually confront your fears in a structured way, starting with situations that cause the least distress and working up to those that are more challenging. The goal is to expose yourself to these situations without engaging in the compulsions or avoidance behaviors that typically follow, allowing your anxiety to naturally decrease over time. This will help you break the OCD cycle so that you are no longer stuck in it.
If you’re also experiencing depression, Ibrahim recommends adding another treatment plan on top of ERP called behavioral activation (BA). “BA is a therapy in which you learn what types of behaviors you’re doing that are feeding the depression and what kind of behaviors you can do that will help you move toward a more positive mood.”
Just like ERP, you’ll create a hierarchy of activities you used to enjoy and activities that you can still do. “It depends on how depressed you are, but if you’re one of those people in bed every day, all day, and you don’t get up, BA looks like getting out of bed, opening your curtains, and brushing your teeth,” says Ibrahim. “That could be at the start of your BA hierarchy.”
In some cases, BA can be implemented to help you start ERP therapy. “When people aren’t motivated to do ERP because their depression is so big, it can help to chip away a little bit of the depression to increase motivation to do ERP.”
If you’re dealing with SAD, a light therapy lamp may help reduce symptoms. However, for OCD, ERP is the most recommended treatment, where light therapy can be added as supplemental therapy. In cases where both OCD and seasonal mood changes like SAD are present, combining light therapy to address mood regulation with ERP for OCD can be an effective approach.
Find the right OCD therapist for you
All our therapists are licensed and trained in exposure and response prevention therapy (ERP), the gold standard treatment for OCD.
Bottom line
Depending on the advice of your healthcare provider, light therapy may be a helpful way to supplement your OCD treatment plan, particularly if you’re experiencing seasonal mood changes or co-occurring conditions like depression. However, it’s important to remember that light therapy shouldn’t replace evidence-based therapies like ERP, which directly target the underlying symptoms of OCD.
Key Takeaways
- Obsessive-compulsive disorder (OCD) symptoms can get worse in the winter as a result of co-occurring mental health conditions such as depression and anxiety.
- Light therapy can’t treat OCD itself, but it can be incorporated in your treatment plan to help you with symptoms of seasonal affective disorder (SAD).
- Exposure and response prevention (ERP) therapy, a specialized form of cognitive behavioral therapy (CBT), is recommended as a first-line treatment for OCD.